5 Ways Treatment Centers Are Using AI to Save Time and Increase Admissions
AI in healthcare revolutionizes how treatment centers deliver care and manage their operations. The technology reshapes clinical decision-making and optimizes operational efficiency in medical facilities.
Automation has reimagined healthcare workflows in hospitals. AI tackles vital challenges that once took up the core team’s time – from predicting patient admissions to optimizing resource allocation. Medical professionals can now focus on patient care because clinical workflow automation handles routine tasks like medical scribing. The technology also helps detect potential health complications early, which allows medical teams to take preventive action and improve patient outcomes.
Royal Reef Media leads efforts to document how treatment centers make use of these technologies. The focus remains on two crucial goals: saving valuable time and increasing patient admissions. This piece explores five specific ways AI delivers these benefits while enhancing patient care quality.
AI-Powered Patient Intake and Triage
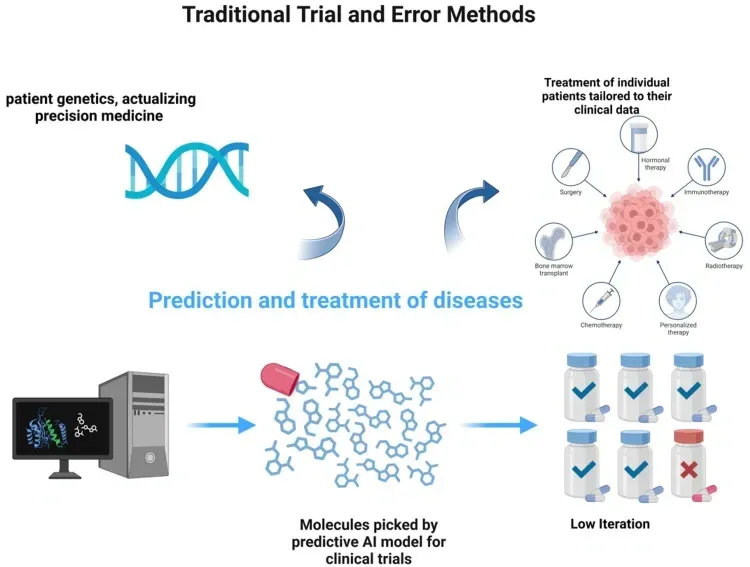
Image Source: AI GPT Journal
Treatment centers nationwide are under pressure to optimize their intake processes. AI-powered patient intake and triage systems have emerged as game-changing tools to tackle these challenges. At Royal Reef Media, we lead research efforts to learn how these technologies transform behavioral health admissions and patient care.
What AI-powered patient intake and triage is
AI-powered patient intake and triage offers a smart approach to process patients. It uses artificial intelligence to collect, analyze, and prioritize patient information before clinical consultations.
AI intake systems help optimize everything for patients, staff, and physicians.
The AI-powered triage does much more than collect data.
These systems don’t try to replace human clinicians – they boost their capabilities instead. A healthcare expert puts it well: “Generative AI is an incredible technology because it’s so adaptable…
How AI-powered patient intake and triage works
AI intake systems combine several advanced capabilities. Natural Language Processing (NLP) sits at the core of many systems.
The AI system connects with patients through various interfaces:
Dynamic interviews: Collects demographic data, symptoms, risk factors, chronic diseases, medications, and medical history Intelligent chatbots: Talk with patients to gather information about pain levels, medical history, and social determinants of health Video and voice assessment: Some systems analyze facial expressions, speech patterns, and response times for a full picture
These systems can find statistical links among patient responses.
Impact of AI-powered patient intake and triage on admissions
AI-powered intake and triage systems bring real improvements to treatment center operations and admission processes.
The administrative benefits stand out too.
AI triage systems excel at predicting which patients will need hospital admission. A study across seven hospital systems looked at records from over 864,000 emergency room visits.
The technology makes things better for patients in several ways:
Patients say AI-driven intake surveys “understood them,” which leads to better participation The systems speak multiple languages and translate medical terms, making them more accessible Patients can complete intake forms remotely, which cuts down waiting room time
AI intake systems help treatment centers dealing with staff shortages. Limbic, which makes clinical AI tools for mental healthcare, has an AI intake agent that can handle unlimited calls at once.
The best part? These systems handle routine intake tasks so clinical staff can focus on providing care instead of pushing paper.
Automated Appointment Scheduling Systems
Image Source: Talkie.ai
Appointment scheduling creates ongoing challenges for treatment centers across the country.
What automated appointment scheduling is
AI-driven automated appointment scheduling brings a digital transformation to the booking process. These systems use artificial intelligence in hospitals to handle appointments with minimal staff involvement. This is a big change from the old way of scheduling through phone calls.
Treatment centers get much more than just digital calendars.
How automated appointment scheduling works
Modern scheduling systems combine several advanced features.
Smart AI programs work behind this user-friendly interface.
- Finding patients with non-urgent needs who could take available times
- Looking at future appointments that could move up
Sending messages through text, email, or app notifications to fill openings
The software also sends automatic reminders.
Impact of automated appointment scheduling on patient flow
AI scheduling brings real improvements to treatment centers.
Patients benefit in several ways:
They can book appointments 24/7, with many doing so after hours (34%, 46%, and 51% of appointments) No more phone tag or hold times leads to happier, more loyal patients Automatic reminders help patients keep their appointments
Modern scheduling systems do more than manage time.
AI in Clinical Decision Support
Image Source: Mount Sinai
Clinical decision support stands at the forefront of AI innovation in healthcare.
What AI clinical decision support is
AI clinical decision support systems are tools that improve healthcare delivery.
These systems help clinicians by analyzing patient data, medical literature, and best practices.
Modern AI clinical decision support uses several advanced technologies:
Machine learning algorithms that recognize patterns and correlations in complex datasets Natural language processing that extracts insights from clinical text and medical records Deep learning models that analyze medical images and sequential data with high precision
These tools process big amounts of healthcare data quickly and accurately. This changes how doctors make treatment decisions in clinical settings.
How AI clinical decision support works
AI clinical decision support combines several advanced components that work together.
The systems start by collecting and analyzing patient information from many sources.
Predictive modeling techniques then assess potential outcomes based on past data.
The process follows these steps:
- Patient data collection and integration with EHR systems
- Analysis using specialized algorithms trained on vast medical datasets
- Generation of personalized recommendations based on evidence and patient-specific factors
- Delivery of useful insights at the point of care
The system’s success depends on how well it fits into clinical workflows.
Impact of AI clinical decision support on treatment accuracy
AI clinical decision support brings real improvements to treatment accuracy and patient outcomes.
AI-driven CDSS helps personalize medicine by analyzing patient records, genetic information, and treatment outcomes from similar cases.
AI systems excel at identifying high-risk patients before their condition worsens.
The technology also improves medication management.
Treatment centers benefit from AI clinical decision support in several ways:
- Better diagnostic accuracy through pattern recognition in complex cases
- Better treatment planning based on evidence and patient-specific factors
- Earlier detection of patient deterioration
- More effective medication management
- Fewer clinical errors and safer patient care
The tools’ usefulness depends on how well healthcare systems implement them.
AI systems show great potential in mental health and addiction treatment diagnosis and planning.
AI-Driven Discharge and Bed Management

Image Source: MedCity News
Bed management continues to be one of the biggest operational challenges that healthcare institutions face today. Royal Reef Media shows how AI in healthcare improves this vital area.
What AI-driven discharge and bed management is
AI-driven discharge and bed management systems predict, optimize, and automate patient movement from admission to discharge. These technologies use machine learning algorithms to forecast bed availability, identify discharge-ready patients, and optimize resource allocation throughout treatment centers.
The platforms combine predictive analytics with automation tools that speed up discharge processes.
The systems keep what experts call “human-in-the-loop” functionality.
How AI-driven discharge and bed management works
The technology behind these systems processes huge amounts of patient data to create accurate predictions.
Developers train the AI on extensive historical data to build effective models.
The process follows this workflow:
- Data collection from multiple sources, including EHRs, admission records, and diagnostic results
- Analysis of historical patterns in patient flow, including seasonal trends and length-of-stay variables
- Live processing of current patient status and facility conditions
- Generation of predictive insights delivered through dashboards and alerts
Staff see these predictions through specialized dashboards in their existing workflows.
These systems excel at spotting subtle data relationships that clinicians might miss.
Impact of AI-driven discharge and bed management on capacity
AI-driven discharge systems bring remarkable improvements to treatment center capacity and resource use. Hospitals report that before AI, they might handle 250 to 300 discharges daily across a region.
- Use beds more efficiently through machine learning optimization
- Cut down overall bed moves by looking at current and future patient needs
Get better patient outcomes through fewer transfers and moves
The benefits go beyond efficiency. Patients recover better at home in familiar surroundings when discharged earlier.
AI-driven discharge and bed management marks a vital step forward in healthcare workflow optimization. It brings clear benefits to patients, providers, and treatment centers alike.
Automation of Administrative Workflows
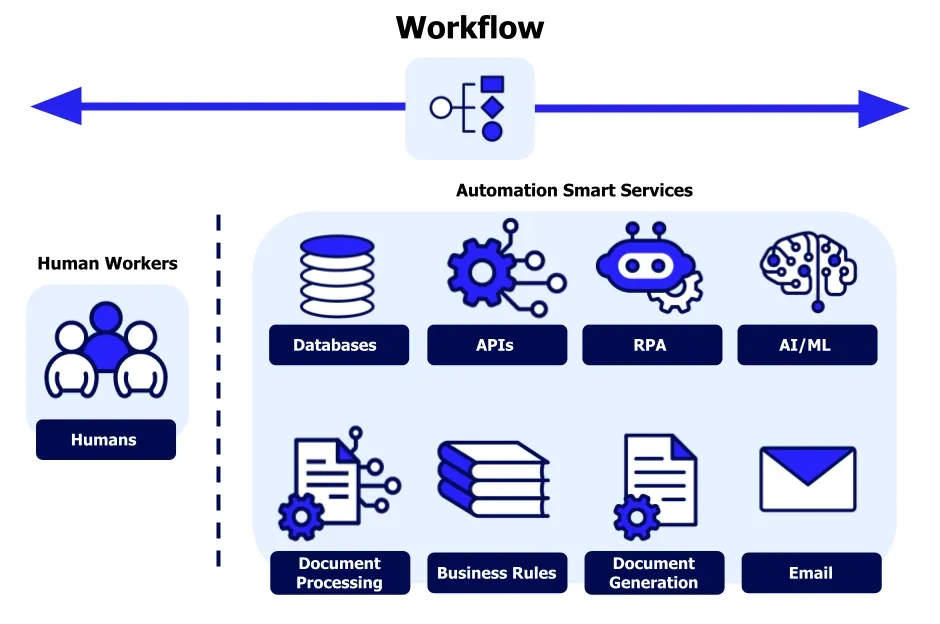
Image Source: Appian
Healthcare professionals spend too much time on administrative tasks.
What administrative automation is
AI technologies help speed up routine administrative tasks in treatment centers. Smart systems handle paperwork, documentation, billing, and other non-clinical processes that overload staff.
Modern administrative automation typically includes:
- Robotic Process Automation (RPA) to mimic human actions in structured tasks like updating records
- Natural Language Processing (NLP) to extract insights from clinical notes
- Machine learning to identify patterns in administrative data
- Integrated workflow management systems that connect clinical and administrative functions
These technologies transform time-consuming manual processes into efficient workflows.
How administrative automation works
The technology combines several advanced components that work together.
The system follows a simple sequence. It collects and analyzes information from various sources, including EHRs and practice management systems. Specialized algorithms identify patterns and make predictions based on historical data. The system then automates actions ranging from simple form completion to complex insurance verification.
Staff adopt these systems more readily when they’re easy to use.
Impact of administrative automation on staff efficiency
Administrative automation brings clear improvements to treatment center operations.
The financial benefits stand out even more.
The benefits go beyond efficiency and help curb burnout. Automation removes tedious data entry and checking tasks.
Comparison Table
| AI Solution | Main Goal | Key Technologies/Components | Implementation Benefits | Reported Impact Metrics |
|---|---|---|---|---|
| AI-Powered Patient Intake and Triage | Automate how patients are processed and prioritized | – Natural Language Processing (NLP) – Dynamic interviews – Intelligent chatbots – Video/voice assessment |
– Fewer data entry errors – Better triage accuracy – Available around the clock |
– 37.5% reduction in visit time (20 to 12.5 minutes) – 85% accuracy in condition identification – 30% fewer data entry errors |
| Automated Appointment Scheduling | Make booking simple and digital | – Cloud-based booking platform – Predictive analytics – Automated reminder system – AI algorithms for pattern analysis |
– Fewer missed appointments – Book appointments anytime – Better use of resources |
– Up to 30% fewer no-shows – 8 minutes saved per patient visit – 15-40% less waiting time and overtime costs |
| AI Clinical Decision Support | Improve diagnosis accuracy and treatment plans | – Machine learning algorithms – Natural language processing – Deep learning models – Predictive modeling |
– More accurate diagnoses – Better treatment planning – Smarter risk assessment |
– 92.8% AUC value for post-stroke pneumonia prediction – 94% success rate in improving clinical practice |
| AI-Driven Discharge and Bed Management | Make patient flow and bed use more efficient | – Predictive analytics – Live processing – Multi-variable analysis (72+ variables) – Dashboard integration |
– Smarter bed allocation – Fewer patient transfers – Prevent bottlenecks early |
– 88% accuracy in 24-hour discharge predictions – Doubled daily discharge capacity (300 to 600) – 17% more accurate forecasting |
| Administrative Workflow Automation | Make routine tasks easier | – Robotic Process Automation (RPA) – Natural Language Processing – Machine learning – Integrated workflow systems |
– Less paperwork – Staff works more efficiently – Better communication |
– 30-60 minutes saved daily per practitioner – $200-360 billion possible savings over 5 years – 47.1% less EHR time at home |
Conclusion
Artificial intelligence shows amazing potential to help treatment centers overcome their operational challenges. The five AI applications we discussed – patient intake systems, appointment scheduling, clinical decision support, discharge management, and administrative automation – have improved efficiency and admissions capacity. The return on investment makes sense through better operations and patient care, despite the upfront costs.
Treatment centers using AI-powered intake systems process patients faster while keeping clinical standards high. Automated scheduling removes phone wait times and reduces no-show rates by up to 30%. Evidence-based recommendations from clinical decision support systems lead to better diagnoses and treatment results.
These benefits reach far beyond one-on-one patient care. AI-powered discharge management helps facilities use beds more efficiently. Some centers have doubled their daily discharge numbers. Staff members spend less time on paperwork thanks to administrative automation, so they can focus more on patients.
Royal Reef Media stays at the forefront of covering these game-changing technologies. Our research proves that AI does more than just improve operations – it makes patient care better. Centers that use these technologies gain an edge through faster processing, better clinical results, and higher admission capacity.
AI in healthcare will become even more sophisticated. Notwithstanding that, today’s technologies already solve many long-standing problems effectively. Treatment centers that smartly adopt these AI tools set themselves up for growth while giving patients exceptional care.
FAQs
Q1. How does artificial intelligence save time in healthcare settings?
AI automates administrative tasks like documentation and scheduling, optimizes clinical workflows, and provides decision support tools. This allows healthcare professionals to spend more time on direct patient care and less on paperwork.
Q2. What are some key applications of AI in treatment centers?
Key AI applications in treatment centers include patient intake and triage systems, automated appointment scheduling, clinical decision support tools, AI-driven discharge and bed management, and automation of administrative workflows.
Q3. How does AI improve treatment outcomes for patients?
AI analyzes patient data to identify patterns, assess risk factors, and provide personalized treatment recommendations. It can enhance diagnostic accuracy, optimize treatment plans, and predict potential complications, leading to better patient outcomes.
Q4. Can AI help increase admissions in treatment centers?
Yes, AI can help increase admissions by streamlining intake processes, optimizing appointment scheduling, and improving bed management. This allows treatment centers to process more patients efficiently and maximize their capacity.
Q5. What impact does AI have on healthcare staff efficiency?
AI significantly improves staff efficiency by automating routine tasks, reducing administrative burdens, and providing decision support. This allows healthcare professionals to focus more on patient care and complex clinical decisions, ultimately enhancing overall productivity.


0 Comments